Полная версия:
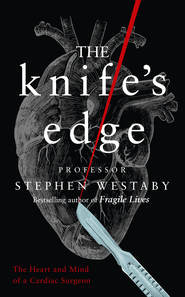
The Knife’s Edge
She whispered, ‘Can you tell mum and dad that I love them, and I’m sorry? They never did want me to have that bike.’
Then she coughed up a plug of blood clot. As she rolled backwards the stake shifted, grating audibly against her shattered ribs. Her eyes rolled towards heaven and she slipped away. Whatever blood she had left in her circulation was pouring out over me. But I didn’t mind. It was a privilege to be there with her. The junior doctors from the resuscitation room stirred, intending to begin cardiac massage. Without hesitation I told them to back off. What the fuck did they expect to achieve?
The back of the ambulance fell silent with the horror of it all. I would have loved to have dragged that hideous fence post out of her chest – that had to be left to the pathologists. I couldn’t bring myself to watch her autopsy, but it confirmed that her diaphragm had been torn away and her pulped liver avulsed from the inferior vena cava.
That balmy summer’s evening I went walking through the bluebell woods of Bladon Heath with Monty, my jet black flat-coated retriever. While he chased rabbits, I sat on a fallen tree carpeted in moss and wondered if there was a God. Where was he on those fraught occasions when I needed some divine intervention? Where was he today when that poor girl tried to avoid hurting a deer and was killed by her kindness? I visualised her devastated parents sitting with a cold corpse in the mortuary, holding their daughter as I’d done in the ambulance, beseeching God to turn the clock back.
There was no point trying to be logical about religion. I knew that high-ranking Oxford – and indeed Cambridge – academics scoffed at the deity concept. Both Richard Dawkins and Stephen Hawking had that gold-plated atheistic confidence in their own abilities, spurning outside help. I guess I was the same. But I would still sneak into the back of a college auditorium and listen to debates on the subject. Some disputed God’s existence because of all the evil and misery in the world, and while I could identify with that, I had contrary and privileged insight through the odd patient who actually claimed to have reached the Pearly Gates before we clawed them back.
These vivid out-of-body experiences were rare but occasionally compelling. One spiritual lady described floating calmly on the ceiling as she watched me pumping her heart with my fist through an open chest. Forty minutes into this internal cardiac massage my thumb tore through into her right ventricle – she clearly recalled my words: ‘Oh shit, we’ve had it now.’ Fortunately, the perfusionists arrived with the circulatory support system I needed to keep her alive, and I succeeded in repairing the hole.
She uncannily related her memory of the events a number of weeks later in the clinic. Having been party to her own resuscitation attempts from above, she had floated through the clouds to meet with St Peter. This journey amid peace and tranquillity contrasted sharply with our gruesome efforts back down on the ground. But having arrived in heaven she was told she had to return to earth and wait her turn again – a ridiculously close-run thing between me and Grim Reaper. Perhaps God changed as he got older. Maybe he started out with the best of intentions but became cynical and less caring with time. Just like the NHS.
It was only after retiring from surgery that I began to reflect on my role in dispatching so many to that great hospital in the sky. One tranquil spot on the heath still holds a great deal of significance for me. It is a haunted place, a gap in the woodland that overlooks both Blenheim Palace, where my hero Winston Churchill was born, and St Martin’s Church, Bladon, where he is buried. A few yards from this clearing a jet plane that had just taken off from Oxford Airport crashed and exploded.
My son Mark was working for exams in his bedroom and watched the whole spectacle unfold. Heroically, he was the first to reach the drama in the field but could do nothing amid the conflagration. He watched the cockpit burn and cremate the occupants. Obviously at seventeen he had a different constitution to his lobotomised father, so the dismal spectacle disturbed him as it might any normal person. After dropping a single grade in biology he was dumped by his chosen university. I was very bitter about that. I still am.
One day when we reached this sacred ground, Monty spotted a stag silhouetted against the evening sky a hundred or so yards up the ride. A shaft of evening sunlight shone through the trees to illuminate a clump of fading bluebells, their heads dipping at the end of their season. Was that majestic stag in fact God looking down on me, surrounded by the spirits I had set free during my career, the ghosts of operations past?
In truth, I had always been a loner. I was still a restless insomniac who would wake in the early hours and write, making stupid notes on material I would never use, continuing to invent impossible operations that no one would ever perform. Did I miss surgery? Not at all, surprisingly enough. Forty years had been plenty. But it remained a great mystery to me how I had achieved so much from my humble beginnings in the backstreets of a northern steel town. Perhaps it was that battle to escape obscurity that provided the momentum. I wanted to be different, and I had the ruthless ambition to take on the system and overcome my past.
Although I spent my whole career writing textbooks and scientific papers for the profession, I reflected for many years on whether it was appropriate to discuss my battles in a public forum. Ironically it was my own patients who urged me to do so, even the loved ones of some who died. So many were eager for their stories to be told. From my own perspective, I always found the history of modern heart surgery to be among the most compelling stories ever told. As a trainee in London and the US I actually knew a number of the pioneers personally, and they had shared their own trials and tribulations with me face to face, encouraging me to make a difference, not to sit in the shadows avoiding conflict. And I certainly attracted trouble right from the start.
The government’s policy of releasing named-surgeon death rates to the press was another factor that edged me towards writing a tome for consumption by the general public. What is life really like on the other side of the fence? Is it different from being a statistician, politician or a journalist? The barrister and medical ethicist Daniel Sokol wrote in the British Medical Journal, ‘The public has an appetite for glimpses of the private lives and thoughts of doctors. They demystify a profession that was once deemed blessed with magical powers.’ Perhaps some of us still do have mystical powers. There are few things more intriguing than delivering electricity into a patient’s head through a metal plug screwed into their skull like Dr Frankenstein’s monster or reinventing human circulation with continuous blood flow without a pulse. These innovations may be construed as witchcraft, but they were my own practical solutions to the terrible illness that is heart failure. Sokol went on to say that doctors are in the habit of revealing ‘not the chiselled frame of Apollo … but the wart covered body of Mr Burns, the Simpsons character’. But Burns was the rich factory owner. I’m more of a sensitive intellectual, like Bart Simpson’s father Homer.
As is often the case, the French have a phrase for it: ‘se mettre à nu’, to get naked. So that is what I decided to do, although this was a much more interesting spectacle in my younger years than now. My own insight tells me that the public are happier to learn that their surgeon, even a heart or brain surgeon, is human and subject to the same core emotions as anyone else. But because of a freak sporting accident, some qualities possessed by the vast majority of people were lost to me for a while, which proved an unexpected but substantial boost to a career at the sharp end – life perpetually on the ‘knife’s edge’.
1
family
When I searched the internet for a contemporary description of the surgical personality, I found this:
Testosterone-infused swagger, confident, brash, charismatic, commanding. Arrogant, volatile, even bullying and abusive. Aggressive. Cuts first, asks questions later, because to cut is to cure and the best cure is cold steel. Sometimes wrong but never in doubt. Good with his hands but no time to explain. Compassion and communication are for sissies.
The psychologist author argued that the highly stressful, adrenaline-fuelled environment in which surgeons work attracts a certain personality type. And so it does. Cutting into people, then wallowing in blood, bile, shit, pus or bone dust is such an alien pastime for normal folk that the mere process of operating immediately sets us apart. Those with introspection and self-doubt select themselves out from my specialty.
It is hard to describe how agonisingly difficult it was to gain access to a cardiac surgery training programme in the 1970s, when open heart surgery with the heart–lung machine was only in its second decade. The surgeons of that era were an unashamedly elitist group with the guts, skill and sheer daring to expose a sick heart and attempt to repair it. Methods to protect the muscle when it was starved of blood were frequently inadequate, and prolonged interaction between blood and the foreign surfaces of the bypass machine triggered a damaging inflammatory reaction known as the ‘post-perfusion syndrome’. Heart surgeons therefore needed above all to work against the clock – deaths were a daily occurrence, yet most patients were so sick that this wasn’t considered a catastrophe. While survival and symptomatic relief were gratifying, death put an end to suffering. Consequently, most families were grateful that their loved ones had at least a chance of their condition improving through surgical intervention.
We all had to go through general surgery training first to show that we had what it takes. First, good hands – and you have to be born that way. Most organs just sit there while you cut and sew them, but the heart is a moving target, a bag of blood under pressure that bleeds torrentially if you bugger it up. Just touching it clumsily can provoke disorganised rhythm and sudden cardiac arrest. Second, the right temperament – the ability to explain death to grieving relatives and to bounce back from a bollocking in the operating theatre. Then courage – the bravery to take over from the boss when he’s had enough, the guts to take responsibility for the post-operative care of tiny babies or to address a catastrophe in the trauma room when the nearest consultant is an hour away. Then patience and resilience – being able to stand there as first assistant for six hours without losing concentration, sometimes with a hangover, or to face five days continuously on call in the hospital, day and night without respite. That was surgical training in those days.
A series of infernal exams to become a fellow of the Royal College of Surgeons was an additional burden over and above the clinical work. These covered every aspect of surgery and only a third of the candidates passed each time. It didn’t matter that I wanted to operate in the chest. For the ‘primary’ fellowship we were required to know the anatomy of a human being in minute detail, brain to asshole, teeth to tits – every nerve, artery and vein in the whole body, where they went, what they did, what happened if we damaged them. We had to learn the physiological processes of every organ and the biochemistry of every cell. After some basic operative experience, the ‘final’ fellowship examined us on the pathology of every surgical condition in the book, then the diagnostic and surgical techniques for each specialty. Only after conclusively demonstrating comprehensive knowledge and skills were we allowed to move on and specialise. I failed both the primary and final fellowship on first sitting, an expensive exercise. Most of my associates did too. The whole miserable process was there to sort the wheat from the chaff, and I wasn’t fazed by failure. It was just like rugby, the sport I loved above all others. Some games you won, others you lost.
The surgical world resembles the army. The consultants are the officers and the gentlemen, the trainees line up in tiers through the ranks: senior house officer is equivalent to corporal, registrar acting as sergeant, senior registrar akin to a non-commissioned officer doing all the work and eventually being promoted to the officer’s mess. That final step was the most competitive of all. For the ruthlessly ambitious it had to be a top teaching hospital. Heart surgeons strove for London hospitals like the Royal Brompton, the Hammersmith, Guy’s or St Thomas’. Appointment to one of these, and you had made it big time. In those days Cambridge had a vibrant cardiothoracic centre in Papworth village out of town. Oxford was doing very little.
All this took place during our formative years, our late twenties and early thirties, when normal people cement relationships, settle down in one location and start a family. Trainee surgeons lived like gypsies, moving from city to city – wherever the best posts were advertised. Something about being a surgeon elevated us to a different plane. We were the fighting cocks of the doctors’ mess, the flash Harrys who constantly strove to outdo each other and ruthlessly coveted the top jobs; the guys – and at that time, as now, it was almost exclusively guys – who stayed in the hospital night after night seeking every chance to operate, or, if it was quiet, drifting across to the nurses’ quarters, where other exciting action was easy to find.
I was a backstreet kid from Scunthorpe who had married his childhood sweetheart from the local grammar school. Caught up in this whirlwind of ruthless ambition, things changed and marriage became an unintended casualty. I was ashamed of this, but I knew some surgical teams where every member, from junior houseman to consultant, was having an affair in the hospital. Grim in reality, but the stuff of television soaps that glamorise adultery. So widespread was the problem that the Johns Hopkins Hospital in Baltimore carried out a formal study of divorce as an occupational hazard in medicine. The younger their residents were when they married, the higher their divorce rate. Understandably, divorce was commonplace when the spouse did not work in the medical field. Blame it on the communication gap. They had little to talk about because doctors – and especially surgeons – are engrossed in their hospital life.
The Johns Hopkins study showed that more than half of psychiatrists and one in three surgeons divorced. Cardiac surgery had an impressive divorce rate, which I already knew from my colleagues’ experience. Reasons cited were high testosterone levels, long hours and nights in the hospital, and close working relationships with numerous attractive young women, often in stressful and emotional circumstances. Professional bonds are formed, and these evolve into romance. At one stage the Dean of Duke University Medical School saw fit to warn applicants that the institution was experiencing a greater than 100 per cent divorce rate. Why exceeding the maximum? Because students showed up already married, got divorced, then remarried and divorced a second time. They all lived a life in which work was seen to come first, with everything else a distant second.
Once at a conference in California I picked up a copy of Pacific Standard magazine that contained an article entitled ‘Why are so many surgeons assholes?’. Obviously it was about prevailing personality types. A scrub nurse friend of the journalist described an incident in the operating theatre where she had passed the sharp scalpel to the surgeon and he lacerated his thumb on the blade. Now furious, he shouted at her, ‘What kind of pass was that. What are we, two kids in the playground with Play-Doh? Ridiculous.’ Then to emphasise his point he threw the scalpel back at her. The nurse was horrified, but as she didn’t know how to react she just kept quiet. No one stood up for her, and no one ever reprimanded the surgeon for being aggressive or throwing the sharp instrument. The inference was that this is how a lot of surgeons behaved and they get away with it all the time.
I have known many surgeons who threw instruments around the room, and although I never aimed one at an assistant I did use to toss faulty instruments onto the floor. It meant that I couldn’t be given them a second time. Having said that, most successful surgeons have certain malign traits in common. These have been summarised in the medical literature as the ‘dark triad’ of psychopathy, Machiavellianism – the callous attitude in which the ends are held to justify the means – and narcissism, which manifests as the excessive self-absorption and sense of superiority that goes with egoism and an extreme need for attention from others. This dark triad emanates from placing personal goals and self-interest above the needs of other people.
Just in the last few months psychologists at the University of Copenhagen have shown that if a person manifests just one of these dark personality traits, they probably have them all simmering below the surface, including so-called moral disengagement and entitlement, which enables someone to throw surgical instruments with absolutely no conscience at all. This detailed mapping of the dark triad is comparable to Charles Spearman’s demonstration a hundred years ago that people who score highly in one type of intelligence test are likely to perform equally well in other kinds. Perhaps the daunting road to a surgical career inadvertently selects characters with these negative traits. It certainly appears that way, yet I had a very different side to my personality when it came to my own family. Maritally I fell into the same old traps, but I would go to any lengths to make my children happy or my parents proud.
I was not rostered to be in surgery as it was my daughter Gemma’s birthday and I hoped to be free. The phantom father who had let her down so many times in the past, I planned to drive to Cambridge in the afternoon to surprise her. Then I discovered that three of our five surgeons were out of town. Two were committed to outreach clinics at district hospitals trying to bring in ‘customers’, as the NHS now called them, or better still the odd private patient. The third was away at a conference, one of those academically destitute commercial meetings at a glamorous resort paid for by the sponsor, with business-class flights and all the rest. As a gullible young consultant I had enjoyed these trips, but it eventually wears thin – tedious airports, buckets of alcohol and forced comradery with competitive colleagues who would cheerfully drive their scalpel into your back the minute it was all over.
It was this surgeon’s operating list that lay vacant, and the unit manager had twisted my arm to stand in for him. To let an operating theatre with a full complement of staff lie idle for the day was a criminal waste of resources, so I reluctantly agreed to the request. I had built this unit from nothing to being virtually the largest in the country, not that anyone could give a shit. The management changed so frequently that history was soon forgotten, dispatched to oblivion by the quagmire of financial expediency. So my daughter would have to wait. Again.
When I asked Sue, my secretary, to find two urgent waiting-list patients at short notice, I didn’t mention the birthday. Just two cases should see me on the road by mid-afternoon. I suggested that one should be the infant girl with Down’s syndrome who had been cancelled twice before. She was in danger of becoming inoperable because of excessive blood flow and rising pressure in the artery to the lungs. I bore special affection for these children. When I started out in cardiac surgery, many considered it inappropriate to repair their heart defects. I couldn’t get my head around a policy that discriminated against kids with a particular condition, so ultimately I overcompensated by taking them on as desperately debilitated young adults – trying to turn the clock back, sometimes without success.
The second case needed to be more straightforward. Sue had repeatedly been pestered by a self-styled VIP who held some snooty position in a neighbouring health authority. When I reviewed this lady in the outpatient clinic, she took exception to my suggesting that weight loss would not only improve her breathlessness but reduce the risks during her mitral valve surgery. I was sternly reminded that she had featured in a recent honours list, presumably for services dedicated to getting her onto an honours list, as is frequently the case in healthcare. I wasn’t in the slightest bit impressed – and she could see that. But she kept insisting on an early date and I couldn’t blame Sue for wanting her out of the way. The titled lady wouldn’t make first slot on the list, however. That was for the baby. A third cancellation was not an option.
6 am. As I set out for work from Woodstock, my home in Oxfordshire, shafts of sunlight burst through the turrets of Blenheim Palace like rays of optimism. I would be seeing Gemma on her birthday. When she was born I was nowhere to be found, and I’d spent twenty years trying to make up for that. Sue, who also suffers from traffic phobia, joined me in the office before 7 am, and we soon dispensed with the paperwork that I had to do before the adult intensive care ward round at 7.30. The day’s operating lists were already displayed on a white board at the main nurse’s station. The male charge nurse knew that my only adult patient was unlikely to reach the unit until mid-afternoon, but still felt obliged to warn me that beds were tight. Glancing towards the row of empty beds surrounded by unplugged ventilators and cardiac monitors, I didn’t need to ask. It was more of the same. ‘Tight on beds’ means not enough nurses. In the NHS, every intensive care bed must have a dedicated nurse. In other countries they double up quite safely to get the work done, but here we just cancel operations as if they were appointments with the hairdresser.
On this particular morning I didn’t know many of the nurses’ faces – and they didn’t recognise me. This told me that the night shift had relied heavily on agency staff. Two of my three cases from the previous day could leave the unit, but only when ward beds became available. Until then, they would continue to languish in this intimidating environment that never slept, at a cost exceeding £1,000 per day. Sometimes we’d even discharge patients directly home from intensive care when the ward was chronically blocked with the elderly and the destitute.
This was not how it used to be. >When we fought to build the department, just three heart surgeons would perform 1,500 heart operations each year and we’d cover the chest surgery between us. Now in the same modest facilities we had five heart surgeons performing half that number of cases, alongside another three chest surgeons operating on the lungs. This was the price of progress – twice as many highly trained professionals doing much less work amid a disintegrating infrastructure. But hey. A hospital delegation was trying to recruit nurses in the Philippines that very week, so all would be well one day.
8 am – and my early-morning optimism was already punctured. I left the cacophony of life support, pulsating balloon pumps, hissing ventilators and screeching alarms. I heard weeping relatives, suggesting that a bed might soon be vacated. Knife to skin should be at 8.30, and I expected the baby to be anaesthetised by now. I assiduously avoided watching parents part from their children at the operating theatre doors. It was traumatic enough for me when my son had his tonsils out. Heart operations were a cut above. When I told parents that their child had a 95 per cent chance of survival, all that registered was the 5 per cent possibility of death. Statistics don’t help when it’s your child that doesn’t make it. So I told them what they wanted to hear, then hoped it would be true.
But the anaesthetic room was empty. The anaesthetist was sitting in the coffee room eating breakfast.
‘Have we sent yet?’ I asked with an air of resignation.

